Definition:
Pinch lower blepharoplasty is a skin-only lower-eyelid procedure in which a narrow strip of redundant skin immediately beneath the lash line is excised by “pinching” the skin to determine a safe amount for removal. There is no skin undermining and the orbicularis oculi muscle and middle lamella are preserved, reducing the risk of lid malposition. It can be combined with transconjunctival fat adjustment and/or resurfacing when needed.
Indications:
Best suited for patients with:
- Mild–moderate lower-lid skin laxity/“crepey” rhytids with good lid tone.
- Minimal or well-controlled fat prolapse, or cases where fat is treated transconjunctivally and the skin excess is addressed with a pinch.
- Fine rhytids where adjunctive laser/peel may be planned.
- Patients desiring a conservative, quick procedure under local anaesthetic with a low risk of ectropion/scleral show compared with skin-muscle flaps.
Contraindications : (relative/absolute)
- Poor lower-lid tone or lax canthus (weak snap-back/distraction test) unless supported with canthopexy/canthoplasty.
- Significant negative vector anatomy with prominent globes and/or marked laxity requiring more extensive support.
- Severe dry-eye disease, lower-lid retraction, cicatricial changes, or previous complicated lower-lid surgery.
- Uncontrolled smokers, anticoagulation that cannot be paused, active thyroid eye disease, infection, or unrealistic expectations.
Advantages:
- Skin-only excision—preserves orbicularis and middle lamella → lower risk of scleral show/ectropion.
- Predictable, conservative skin reduction ; easy to stage/repeat if needed.
- Compatible with adjuncts: transconjunctival fat contouring, canthopexy, and resurfacing.
- Efficient and well-tolerated under local anaesthetic in clinic settings.
Limitations:
- Does not correct significant fat herniation, deep tear-trough/ORL tethering, or malar descent by itself—these may need transconjunctival fat excision/reposition, ORL release, fat grafting, and/or canthopexy.
Limited role in marked laxity or poor canthal support where skin-muscle flaps or canthal procedures are preferred.
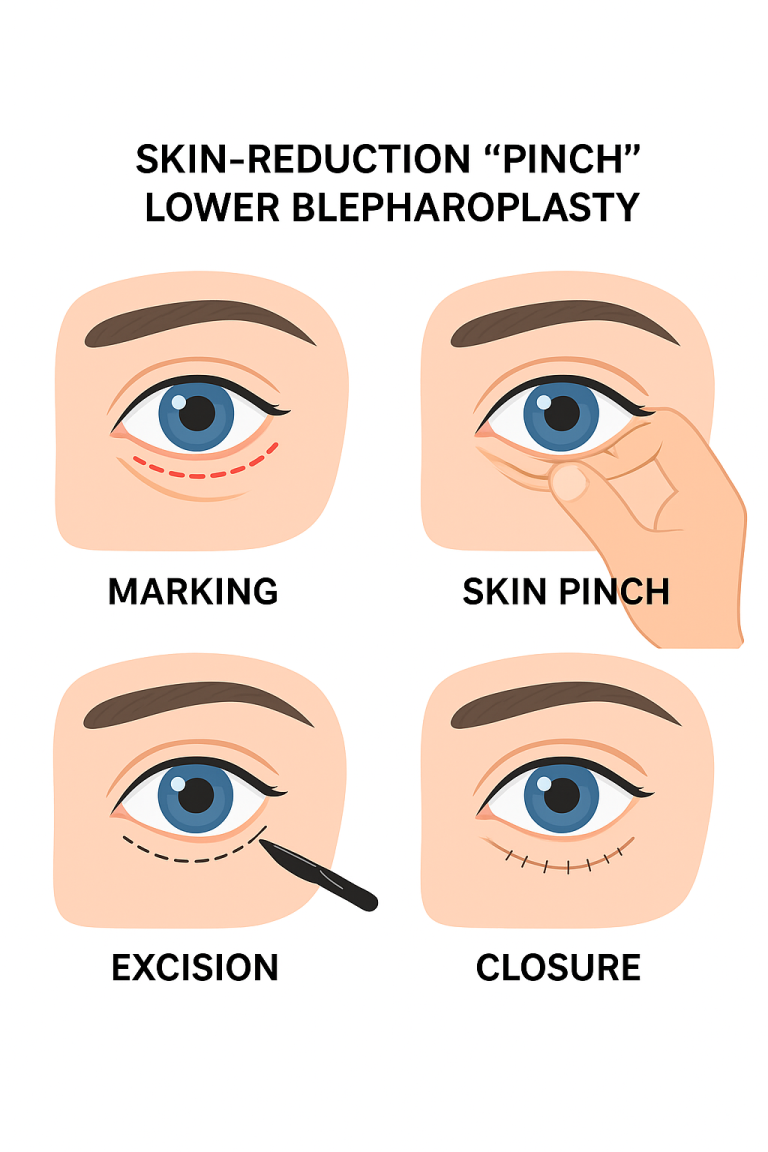
How the procedure is performed :
- Pre-op marking by pinch while the patient looks up; only the skin that comfortably coapts is marked (typically a few millimetres).
- Local anaesthetic infiltration in the subcutaneous plane; sedation or general anaesthesia (GA) are options if needed.
- Subciliary skin ellipse excised without undermining; orbicularis preserved.
- Adjuncts as indicated: transconjunctival fat excision/reposition, lateral canthopexy/canthoplasty, resurfacing.
- Fine interrupted/continuous closure along the lash line; ointment applied.
Anaesthesia options at MACS Clinic
- Preferred: Local anaesthetic (LA) only—highly suitable for isolated skin laxity; rapid recovery.
- LA + light sedation: For patient comfort and/or combined procedures.
- General anaesthesia: For selected combined cases (e.g., extensive fat work or when adding canthal procedures).
Potential risks & complications (not exhaustive)
- Bruising, swelling, mild oozing, temporary numbness/tingling.
- Under- or over-resection of skin; asymmetry; palpable suture tracts; milia.
- Dry-eye symptoms, chemosis (usually transient); irritation from ointments.
- Scarring along the subciliary line (typically fine and fades).
- Lid malposition (retraction, scleral show, ectropion)—risk is lower than with skin-muscle flaps but can occur, especially with poor lid tone; mitigated by canthopexy when indicated.
- Infection, haematoma, delayed wound healing (higher with smoking), pigment change after resurfacing, need for revision.
- Very rare: retrobulbar haemorrhage/vision threat (emergency).
Post-operative care
- Cold compresses 10–15 min hourly for the first 24–48 hours; head elevation for 3–5 nights.
- Lubricant drops/ointment as advised; avoid rubbing.
- Analgesia: paracetamol/ibuprofen if suitable; avoid aspirin unless prescribed.
- Wound care: thin smear of antibiotic/ocular ointment for several days.
- Activity: gentle walking from day 1; avoid strenuous exercise/heavy lifting for ~2 weeks.
- Make-up/camouflage: usually after day 7–10 when the incision is sealed.
- Suture removal (if non-absorbable) typically 5–7 days.
- Sun protection from day 1; silicone/ scar massage from ~3–4 weeks if advised.
- Follow-up at 1 week, 6 weeks, and 3–6 months (or as instructed).
Contact MACS Clinic
Phone: 020 7078 4378
WhatsApp: 07792 648 726
Email: enquiries@macsclinic.co.uk
Website: macsclinic.co.uk







