🧬What Are Secondary Malar Bags (Festoons)?
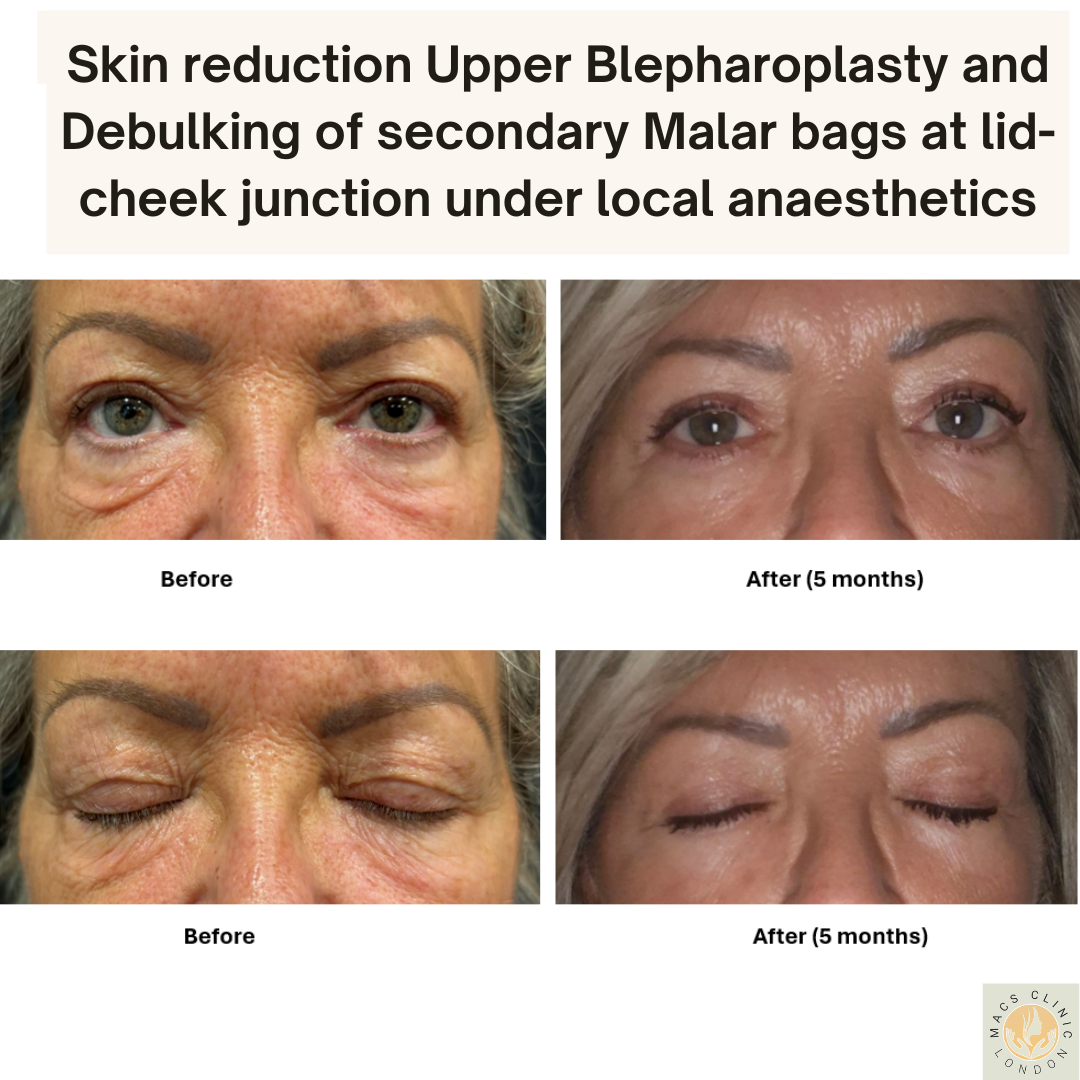
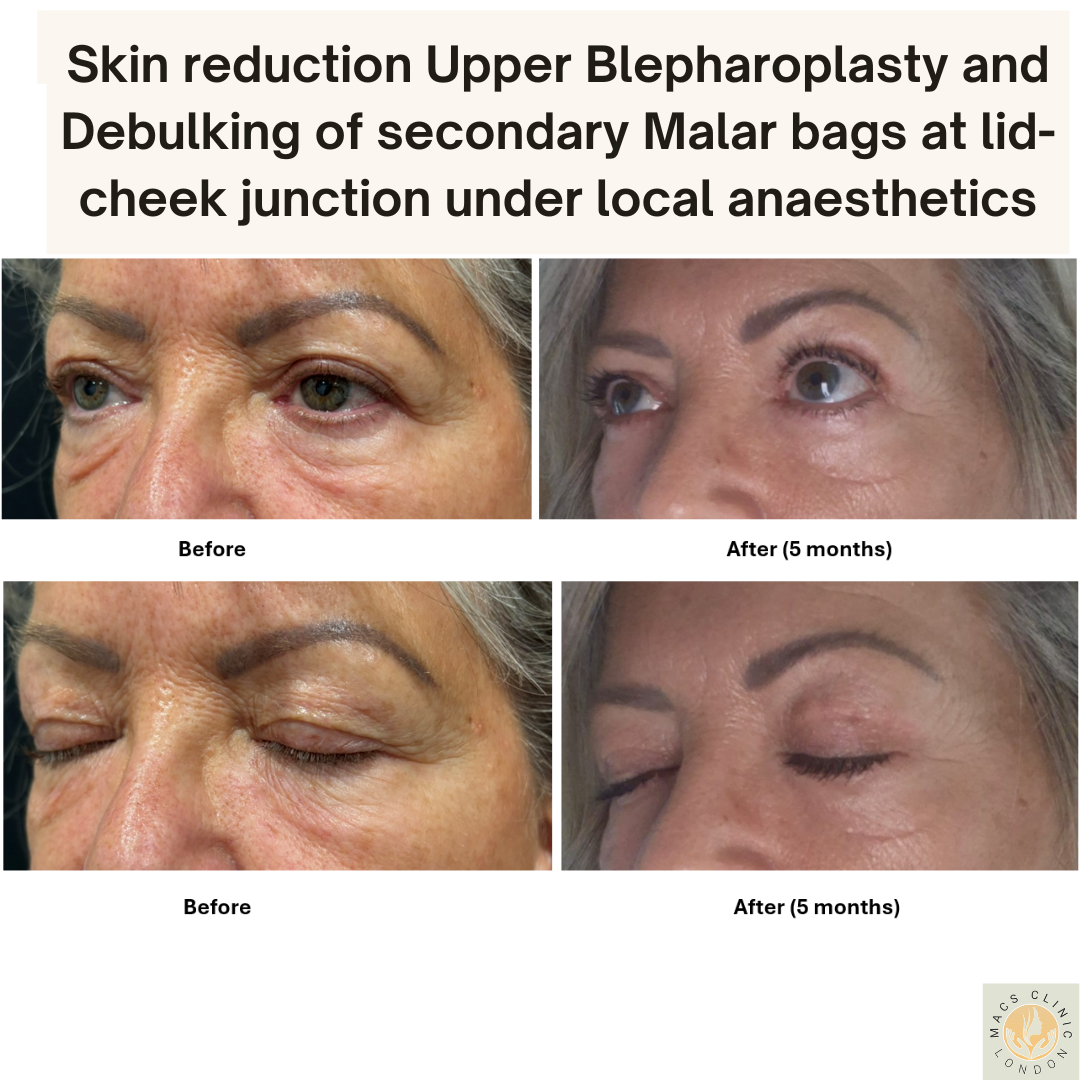
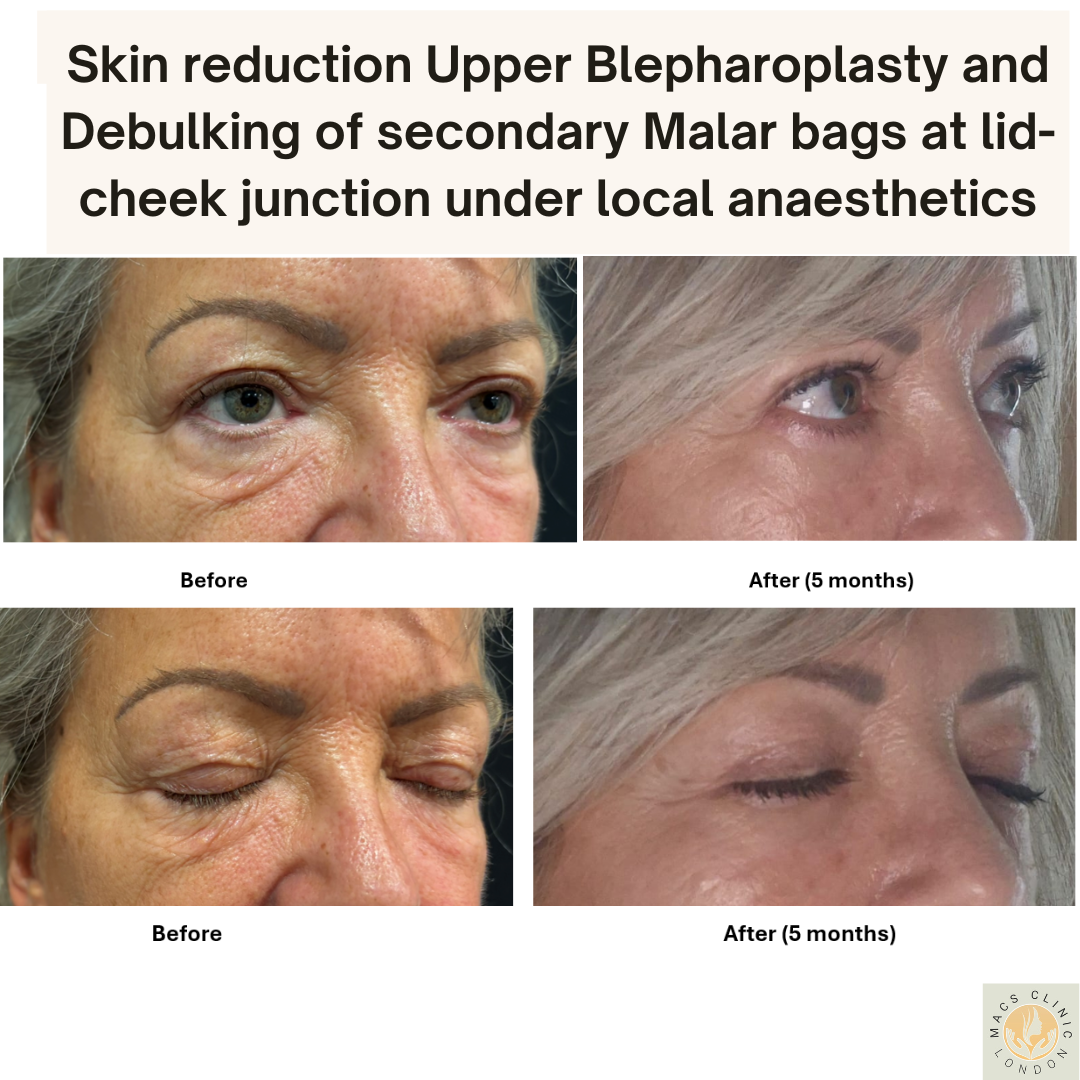
“Secondary malar bags” — medically known as festoons — are persistent swellings or pouches that form just below the lower eyelids, along the upper cheek (malar) area. They are distinct from traditional under-eye bags, which occur closer to the lash line. Festoons often appear as sagging folds or “pouches” over the cheekbone, and they can be resistant to standard cosmetic treatments.
Even when patients are well-rested and hydrated, festoons tend to remain, often worsening over time and contributing to a tired, aged, or swollen appearance.
🔍Common Synonyms
Secondary malar bags are also known as:
Festoons
Malar mounds / malar pads
Malar puffiness / malar pouches
Cheek festoons / cheek pouching
Malar edema / lid-cheek festoons
⚠️Causes & Contributing Factors
Festoons are typically caused by a combination of structural, physiological, and lifestyle factors. Common causes include:
🧬 Age-related tissue changes: Loss of collagen and skin elasticity, combined with gravitational descent of the mid-face.
💉 Previous eyelid surgery: Secondary festoons often appear following lower blepharoplasty due to altered tissue support.
💧 Lymphatic stasis: Reduced lymphatic drainage leads to chronic swelling and tissue congestion.
🩹 Scar tissue or fibrosis: Post-surgical or post-inflammatory changes can produce dense, resistant tissue in the malar area.
☀️ Sun damage: Chronic exposure accelerates skin ageing and tissue breakdown.
🩺 Genetic predisposition: Some individuals are naturally prone to malar puffiness.
🍷 Lifestyle factors: Smoking, alcohol consumption, allergies, and sinus issues can aggravate festoon formation.
🩺 Clinical Diagnosis
A thorough consultation and examination help distinguish festoons from other causes of lower facial swelling, such as:
Orbital fat prolapse (eye bags) – higher position, closer to lash line.
Mid-face ptosis – diffuse descent of cheek tissue.
Allergic or fluid retention-related swelling – fluctuating and softer.
Excess skin (dermatochalasis) – skin laxity without pouching.
Assessment often includes pinch testing, dynamic evaluation, and analysis of the skin–muscle–fat interface.
💉 Treatment Options
Festoons can be challenging to treat, and management is best tailored to each patient. A combination approach is often required for optimal results.
1. 🌿 Non-Surgical & Minimally Invasive Options
These approaches can offer subtle improvement but are usually insufficient for established festoons:
Topical therapies: Retinoids and firming creams improve skin texture but cannot address deeper causes.
Energy-based treatments: Radiofrequency or laser skin tightening enhances surface tone but does not remove fibrotic festoon tissue.
Dermal fillers: Volume replacement around the mid-face can camouflage festoons by improving contour transitions.
Autologous fat transfer: Adds volume and support, often as an adjunct to other treatments.
Lymphatic therapies: Manual drainage or microneedling may help mild, fluid-dominant festoons.
2. ✂️ Direct Multi-Stage Serial Excision (Elliptical Excision)
For well-established or fibrotic secondary festoons, direct multi-stage serial excision remains one of the most effective, reproducible, and predictable treatments.
Key features:
✅ Performed safely under local anaesthetic as a day-case procedure.
✅ Minimal downtime — most patients resume daily activities within a few days.
✅ Involves carefully staged removal of excess fibrotic tissue using elliptical excisions, often over 2–3 sessions.
✅ Cost-effective — significantly less expensive than a mid-face lift or major surgical alternative.
✅ Reproducible outcomes with steady improvement after each session.
Scar maturation:
As with any excisional procedure, a fine linear scar remains in the treated area. This scar typically softens, flattens, and becomes less noticeable over a period of 18 months to 2 years as it matures. Patients are advised to camouflage the healing scar with foundation cream or suitable makeup during the recovery phase. In most cases, the scar blends naturally into the skin over time.
3. 🪄 Mid-Face Lift (Cheek Lift)
A mid-face lift, also known as a malar or cheek lift, repositions descended cheek tissues and improves festoon appearance by tightening and elevating the mid-face.
Best suited for: Patients with significant cheek descent or combined festoon and mid-face laxity.
Approaches: Endoscopic, subciliary, or transconjunctival.
Advantages: Addresses deeper structural issues.
Limitations: Greater cost, longer downtime, and more invasive.
⚖️ Limitations of Treatment
While major aesthetic improvements are achievable, complete eradication of festoons may not always be possible. Residual effects may occur due to:
Deep fibrosis or scar tissue
Chronic lymphatic dysfunction
Underlying skeletal or soft-tissue structure
Individual healing variability
Realistic expectations and a staged treatment plan are essential for optimal outcomes.
⚠️ Possible Complications
When performed by a qualified aesthetic surgeon, treatment for festoons is generally safe. However, potential risks include:
Swelling and bruising
Minor asymmetry or contour irregularities
Scar changes (rarely significant)
Infection (rare)
Temporary numbness or altered sensation
Incomplete correction or recurrence
🧠 Key Takeaways
Festoons (secondary malar bags) are one of the more complex mid-face ageing features but can be successfully treated.
Non-surgical methods provide modest improvement and are best for early cases.
Direct multi-stage serial excision is a highly effective, low-downtime, and cost-efficient solution with reproducible results under local anaesthetic.
Mid-face lift and volumising procedures (fillers or fat transfer) may be added for comprehensive rejuvenation.
Realistic expectations and a personalised plan are crucial to satisfaction.
Contact MACS Clinic
- Phone: 020 7078 4378
- WhatsApp: 07792 648 726
- Email: enquiries@macsclinic.co.uk
- Website: co.uk
BOOK a FREE Video Consultation: https://calendly.com/macsclinic/free-video-consultation?month=2025-01







