Hypertrophic scars and keloids are two types of thickened scars that can form after injury, infection or surgery. Both result from an overproduction of collagen during the healing process, but they differ in appearance and behaviour.
Hypertrophic scars
Hypertrophic scars are raised, thickened areas of skin that develop after an injury, infection or surgery. Unlike keloids, hypertrophic scars remain within the boundaries of the original wound and do not spread to surrounding skin. They are a result of excessive collagen production during the healing process.
Causes of Hypertrophic scars
- Injury or Surgery: Cuts, burns, piercings, or surgeries that damage the skin can lead to hypertrophic scarring.
- Excess Tension: Scars that form over joints or areas of high movement are more likely to thicken due to the skin’s constant stretching.
- Infection or Inflammation: Prolonged inflammation or infection during wound healing can trigger an overactive healing response, leading to thickened scars.
Symptoms of Hypertrohic scars
- Raised and Firm: Hypertrophic scars are raised, but they usually stay within the boundaries of the original wound.
- Red, Dark or Light: These scars can appear reddish, pink, or darker than the surrounding skin.
- Itching or Sensitivity: They may cause mild discomfort, itching, or sensitivity during the healing process.
Aesthetic Compromises due to Hypertrophic scars
Hypertrophic scars can affect the appearance of the skin, especially in visible areas like the face, neck, or hands. Though they may flatten and fade over time, they often leave a noticeable raised mark that can cause self-consciousness or dissatisfaction with one’s appearance.
Effect on Social Life due to Hypertrophic scars
While hypertrophic scars are not typically harmful, their appearance can impact an individual’s confidence and social interactions. People with noticeable scars may feel self-conscious in social situations, which can affect their overall emotional well-being and social life.
Keloids
Keloids are a type of raised scar that form as a result of excessive collagen production during wound healing. Unlike hypertrophic scars, keloids extend beyond the original wound boundaries and can continue to grow over time, forming a thick, raised mass of scar tissue. They often become larger than the original injury and can affect any part of the body, though they are more common on the chest, shoulders, earlobes, and cheeks.
Causes of Keloids
- Genetics: Keloids are more common in people with darker skin tones, such as African, Hispanic, or Asian populations. A family history of keloids increases the likelihood of developing them.
- Injury or Trauma: Keloids can form after skin injuries, including cuts, surgical incisions, piercings, acne, burns, and even minor wounds like insect bites or scratches.
- Infection or Inflammation: Prolonged inflammation or an infection during wound healing may trigger keloid formation.
Symptoms of Keloids
- Raised, Lumpy Appearance: Keloids are thick, firm, and often larger than the original wound, extending beyond its boundaries.
- Discoloration: They can appear red, pink,darker or lighter than the surrounding skin.
- Itching and Pain: Keloids may cause discomfort, itching, tenderness, or even pain, particularly as they grow.
- Slow Growth: Keloids can grow slowly over months or even years after the initial injury.
Aesthetic Compromises due to keloids
Keloids are often noticeable and can lead to significant cosmetic concerns, especially when they occur on visible areas like the face, neck, or ears. Their raised, bulky appearance can affect the skin’s natural contour, making them aesthetically unappealing to some individuals.
Effect on Social Life due to keloids
The prominent appearance of keloids can lead to emotional and psychological distress. People with visible keloids may feel self-conscious, leading to a decrease in self-esteem and social engagement. In some cases, the presence of keloids can affect one’s willingness to participate in activities where scars may be exposed, such as swimming or wearing certain type of clothings.
How to treat Thickened scars at MACS Clinic
Thickened scars, such as hypertrophic scars and keloids, are common after procedures like face lift, gynecomastia correction, abdominoplasty, breast augmentation, breast reduction, split ear lobule repair and prominent ear correction etc. While post-operative care is crucial in preventing these scars, they may still occasionally develop despite best efforts. Mr. Shailesh Vadodaria provides his patients with a detailed post-operative care instruction leaflet to minimize the risk of scar formation. However, when thickened scars do occur, they require timely and appropriate treatment as follows:
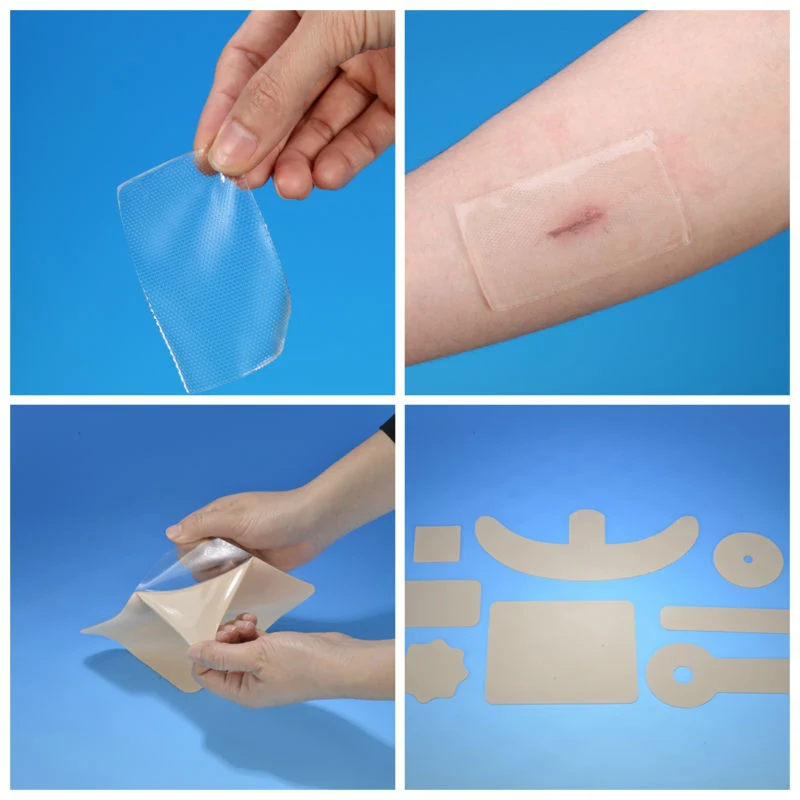
Pressure Therapy
Special pressure garments or silicone sheets are used to flatten the scar and reduce its size. This is mostly recommended by Mr. Vadodaria in early stages, particularly for hypertrophic scars. Consistent use is required over several months. Pressure therapy is recommended by Mr. Vadodaria after gynecomastia, brachioplasty, breast reduction, breast augmentation etc procedures to avoid the formation of thickened scars.

Moisturizers
Keeps the scar tissue hydrated and prevents further thickening. It helps to reduce dryness and itching, promoting smoother skin texture. Bio-Oil, Nivea cream, and E45 are good moisturizers to prevent/treat thickened scars

Massage
Massaging the scar tissue gently can break down excess collagen and improve the flexibility of the skin. Regular massage may reduce stiffness and flatten raised scars over time
Steroid Injections
These are used to shrink keloids and hypertrophic scars by reducing inflammation and collagen production. This is often a first-line treatment and can significantly reduce the size and discomfort of the scar.
Surgery
Surgical removal of the scar can be an option, though it carries the risk of recurrence, especially for keloids. Post-surgical recurrence of keloids is common, so surgery is often paired with other treatments like steroid injections or radiotherapy.
Radiotherapy and Surgery
Low-dose radiation therapy following surgical removal of a keloid can prevent regrowth by targeting the cells responsible for excessive collagen production. This combination can be effective, but radiotherapy is typically reserved for severe or recurrent keloids due to potential side effects.
Pressure Clips for Ear Lobule Keloid
Pressure clips are a non-invasive treatment option used by Mr. Vadodaria specifically designed for keloids on the ear lobule. These clips apply constant pressure to the keloid, helping to flatten and reduce its size over time. Pressure clips are often custom-made to fit the shape and size of the earlobe, ensuring effective pressure is applied without causing discomfort.
Pressure clips are most effective when used in the early stages of keloid formation or immediately after keloid surgery to prevent recurrence. The clip needs to be worn for extended periods, often up to 12-16 hours a day, for several months.
Pressure clips are a useful, low-risk option recommended by Mr. Vadodaria for treating or preventing keloids on the earlobes, especially after a split ear lobule repair and ear lobe reduction.
In conclusion, scar management after surgery requires a combination of general guidelines and personalized care based on the specific procedure performed. By adhering to post-operative instructions and attending regular follow-ups with Mr. Shailesh Vadodaria, patients can appropriate advise to minimise chances of abnormal scar formations and manage the symptoms and signs of hypertrophic scar and keloid following surgery, injury or infection. Patience and consistency are essential, as scar healing is a gradual process.
To know more about Scar Management After Surgery At MACS Clinic visit: https://macsclinic.co.uk/scar-management-after-surgery-at-macs-clinic/
Contact Us
call us
02070784378
Email Us
info@macsclinic.co.uk
Opening Hours
9:30 AM - 6:00 PM
Visit Us
www.macsclinic.co.uk







