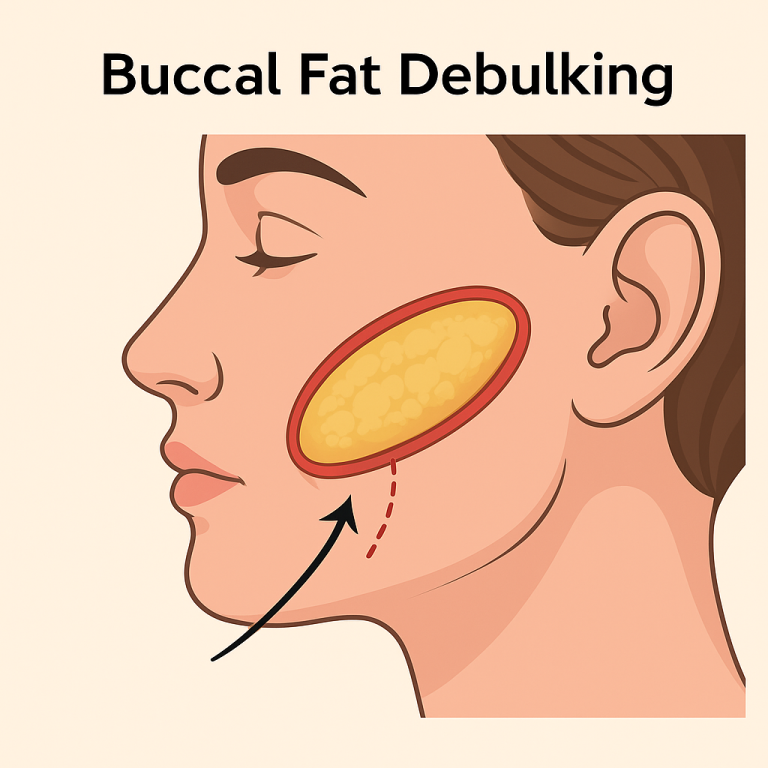
1) What is buccal fat debulking?
Buccal fat debulking is a minor surgical procedure to reduce the buccal (cheek) fat pad through a small incision inside the mouth. It aims to reduce volume of buccal fat making a cut in the cheek mucosa in from inside the mouth. The outer skin has no external scars.
2) Who might benefit? (Indications)
- Persistent mid-cheek fullness despite healthy weight and lifestyle.
- Desire for subtle, natural debulking to improve cheek definition (not a jawline/jowl procedure).
- Stable body weight (as weight fluctuation changes facial fullness).
- Realistic expectations about modest, gradual contouring (final contour becomes clearer once swelling settles which takes upto 18 to 24 months).
Important on timing & ageing
- The buccal fat pad commonly atrophies spontaneously after 30 years , contributing to a naturally slimmer mid-face with age.
- Therefore, caution is advised in patients approaching this age range or those with naturally thin faces; over-resection can cause premature gauntness as ageing progresses.
3) Who should avoid it? (Contraindications)
- Very thin faces or established mid-face deflation / strong hollowing tendency.
- Ageing concerns where future volume loss is likely to accentuate hollows.
- Unrealistic expectations (desiring dramatic changes or a jawline lift effect).
- Poor oral hygiene, active dental/sinus/oral infections, active mouth ulcers.
- Bleeding disorders, uncontrolled hypertension, or use of anticoagulants/antiplatelets (unless safely managed).
- Heavy smokers or vapers (impaired healing risk).
- Body dysmorphic disorder or significant untreated psychological concerns.
- Recent major weight change (wait until weight stabilises).
4) Alternatives to consider
- Weight optimisation and lifestyle measures.
- Botulinum toxin to masseters (if bulk is muscular rather than fatty).
- Skin tightening (for skin laxity; does not remove fat).
- Midface/cheek augmentation (implants or fillers) if the issue is lack of projection rather than excess fat.
- Fat grafting to balance contours elsewhere rather than remove buccal fat.
- Doing nothing and reassessing after natural age-related buccal fat atrophy.
5) Where is the incision and what is protected?
- A 1.5–2 cm incision is made inside the cheek, usually opposite the upper second molar.
- The surgeon carefully protects the parotid (Stensen’s) duct opening in this area and avoids the branches of the facial nerve (which run more superficially outside the cheek but can be affected indirectly by deep dissection, thermal injury or inflammation).
- Only the buccal extension of the buccal fat pad is conservatively removed to avoid hollowing.
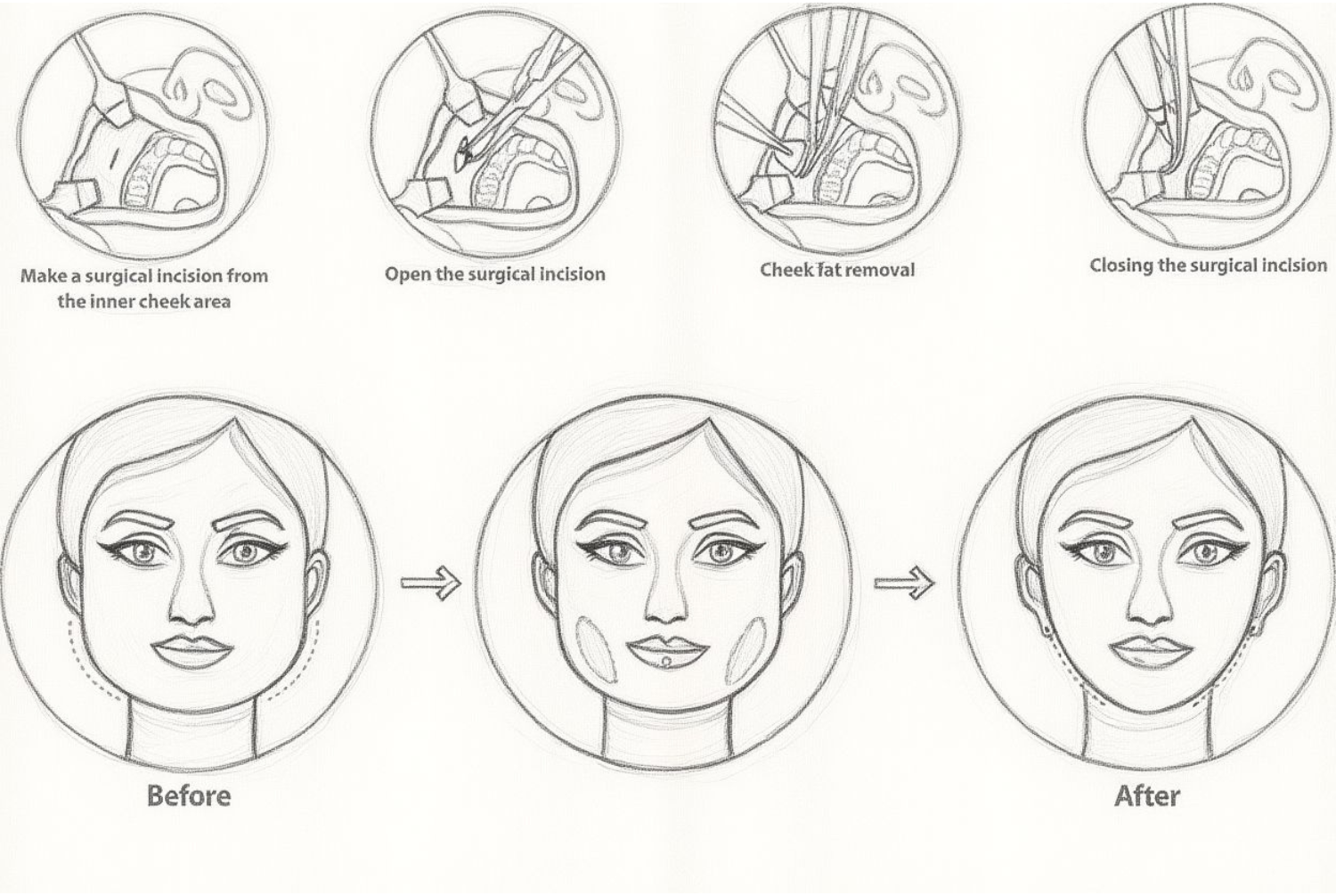
6) How is the procedure done? (Outline of technique)
- Anaesthetic: Local infiltration with or without IV sedation, or General anaesthetic (see below).
- Antiseptic oral rinse and sterile preparation.
- Small intra-oral incision through mucosa and buccinator muscle fibres.
- Gentle, blunt delivery of the buccal fat pad; conservative debulking only.
- Meticulous haemostasis.
- Closure with resorbable stitches (no removal needed).
- External cold compresses are used for early swelling control.
Duration: ~30–45 minutes for both sides (variable).
Setting: Day case — patients go home the same day.
7) Anaesthetic options
- Local anaesthetic (LA) only: Numbs the cheeks; quickest recovery; suitable for many patients.
- LA + IV sedation: Adds relaxation/drowsiness; you remain rousable; someone must escort you home.
- General anaesthetic (GA): Asleep for the procedure; usually chosen if combining with other procedures.
Your anaesthetic plan is tailored to your health, comfort, and any combined procedures.
8) Recovery & aftercare
- Swelling & bruising: Common for 1–2 weeks
- Discomfort: Usually mild–moderate; oral analgesics as directed.
- Diet: Soft, cool diet for several days; avoid spicy, acidic, or hard/crunchy foods that irritate the incision.
- Mouth care: Antiseptic mouthwash as prescribed (e.g., chlorhexidine), gentle salt-water rinses after meals, careful brushing away from the incision lines.
- Activity: Head elevation for 48 hours; avoid strenuous exercise, hot environments, and heavy lifting for ~1–2 weeks.
- Smoking/vaping: Strictly avoid (healing risk).
- Follow-up: Typically at ~1 week and again at 6–12 weeks, or as advised.
9) Risks & possible complications
While complications are uncommon, you should understand and accept the following possibilities:
Common/expected
- Swelling, bruising, temporary tightness, mild pain.
- Limited mouth opening (trismus) for a few days.
- Transient numbness of the cheek mucosa.
Early complications
- Bleeding/haematoma, prolonged oozing.
- Infection or delayed wound healing inside the mouth.
- Salivary issues:
- Injury or irritation of the parotid (Stensen’s) duct causing salivary leak, sialocele or duct stenosis (may require massage, aspiration, botulinum toxin to gland, or rarely further intervention).
- Injury or irritation of the parotid (Stensen’s) duct causing salivary leak, sialocele or duct stenosis (may require massage, aspiration, botulinum toxin to gland, or rarely further intervention).
- Nerve irritation:
- Sensory change (inner cheek numbness/tingling).
- Facial nerve (buccal branch) weakness is rare with an intra-oral approach but possible via deep thermal injury, traction, or inflammation — may cause temporary cheek movement weakness; very rarely persistent.
- Sensory change (inner cheek numbness/tingling).
Aesthetic/late complications
- Asymmetry or contour irregularity.
- Over-resection leading to hollowing/gauntness and prematurely aged appearance (may need fat grafting or fillers later).
- Under-correction (residual fullness), sometimes needing staged revision.
- Scar tissue inside the mouth, persistent tightness, or prolonged swelling.
- Unmasking of skin laxity or jowls (procedure does not tighten skin).
- Effect altered by future weight change or natural ageing.
Anaesthetic-related risks depend on the method used and your medical history and will be discussed with you.
10) Limitations — what buccal debulking does not do
- It does not lift or tighten the jowls, jawline, or neck.
- It does not replace weight control or address masseter muscle hypertrophy (that may need botulinum toxin).
- The change is subtle-to-moderate, aiming for refinement rather than dramatic transformation.
- Ageing continues; future volume loss can increase cheek hollowing over time.
11) Possibility of revision surgery
- Results are assessed after swelling settles
- If there is under-correction or asymmetry, a staged revision may be discussed.
- If over-resection or hollowing occurs, treatment options include fat grafting or hyaluronic acid fillers to restore volume.
- Any revision carries additional risks, downtime and costs, which will be explained if relevant.
12) Preparation checklist (before your procedure)
- Maintain excellent oral hygiene; complete any pending dental work first.
- Stop smoking/vaping as advised.
- Disclose all medications, supplements, and allergies (especially blood thinners/NSAIDs/herbals).
- Arrange a responsible adult escort if you are having sedation or GA.
- Maintain a stable weight for several weeks prior.
- Have realistic goals; review before/after examples and limitations with your surgeon.
13) Summary for consent
- Buccal fat debulking is performed from inside the mouth as a day-case under local anaesthetic ± sedation or general anaesthetic.
- It offers modest cheek refinement; final results need complete maturation of scar
- Key specific risks to understand:
- Injury to the parotid (Stensen’s) duct (salivary leak/stenosis).
- Branches of the facial nerve (rare weakness).
- Over-resection with hollowing and asymmetry/irregularity.
- Injury to the parotid (Stensen’s) duct (salivary leak/stenosis).
- Natural buccal fat atrophy commence at around 30 years means cautious patient selection is essential to avoid gauntness with ageing.
Revision may occasionally be required.
Contact MACS Clinic
- Phone: 020 7078 4378
- WhatsApp: 07792 648 726
- Email: enquiries@macsclinic.co.uk
- Website: co.uk
BOOK a FREE Video Consultation: https://calendly.com/macsclinic/free-video-consultation?month=2025-01







